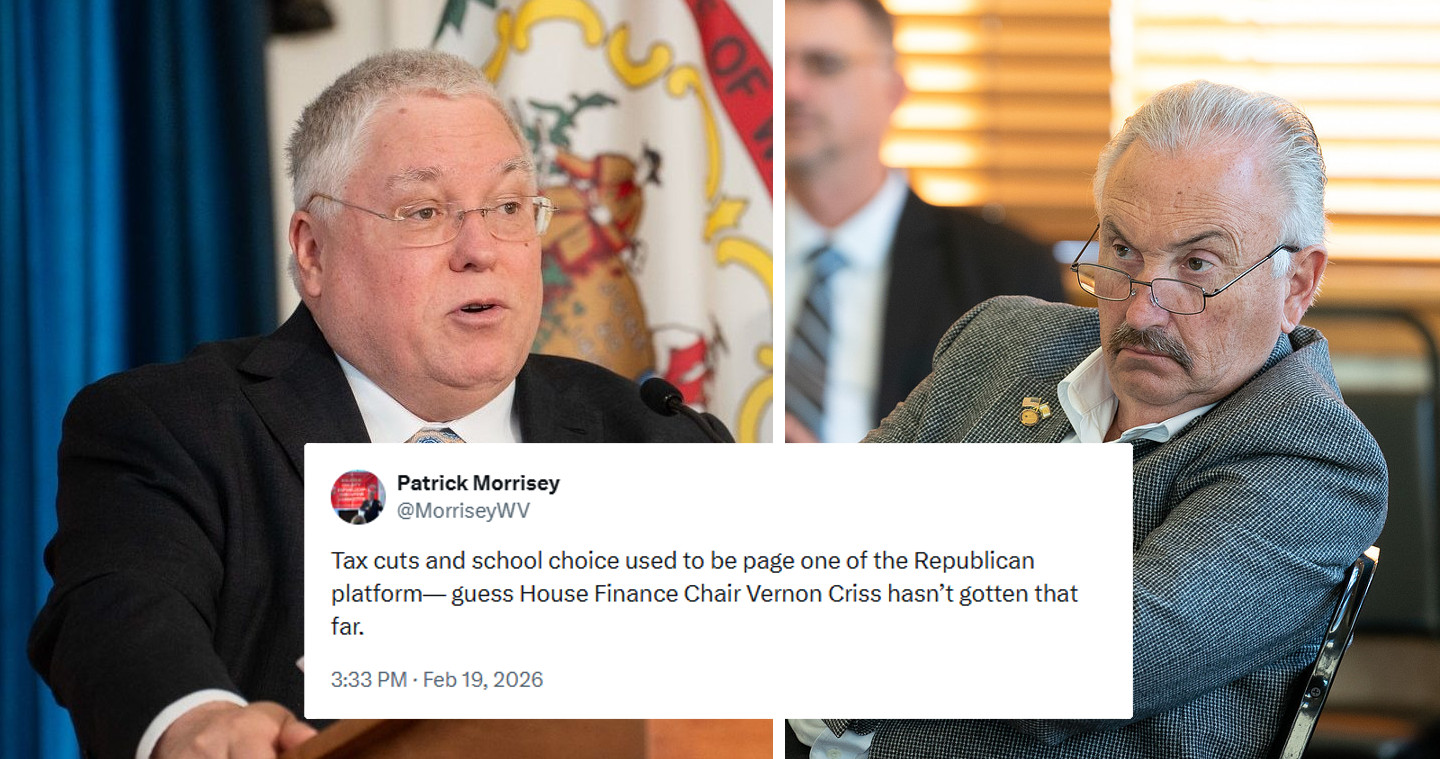
CHARLESTON — As one of his last acts serving as the West Virginia’s Attorney General, Patrick Morrisey announced that a settlement has been reached with Tiero, a Delaware-based company accused of improperly billing the state’s Medicaid program for at-home COVID-19 test kits.
Morrisey said Tiero’s claims for reimbursement were invalid because the company was not enrolled as a Medicaid provider at the time of billing. Tiero had submitted claims using a billing code designated for antigen testing services, which Morrisey stated was inaccurate for the products in question.
“Healthcare providers must ensure they use the correct billing codes and only bill for services that are medically necessary,” said Morrisey. “Any provider wishing to do business with the Medicaid program must be properly enrolled and comply with all regulations.”
The settlement requires Tiero to pay full restitution of $439,000 to the state.
Morrisey praised his office’s Medicaid Fraud Control Unit (MFCU) for its efforts in uncovering the fraudulent claims. He specifically commended Investigator Kelley Mitchell, Fraud Analyst Brooke McArdle, and Attorney Stephen Kenney for their work on the case, which led to the successful resolution.
The settlement serves as a reminder of the state’s commitment to holding healthcare providers accountable for ensuring proper billing practices in the Medicaid system.